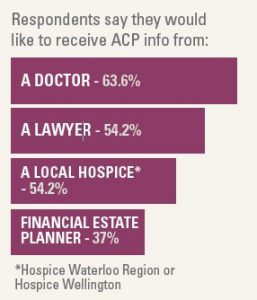
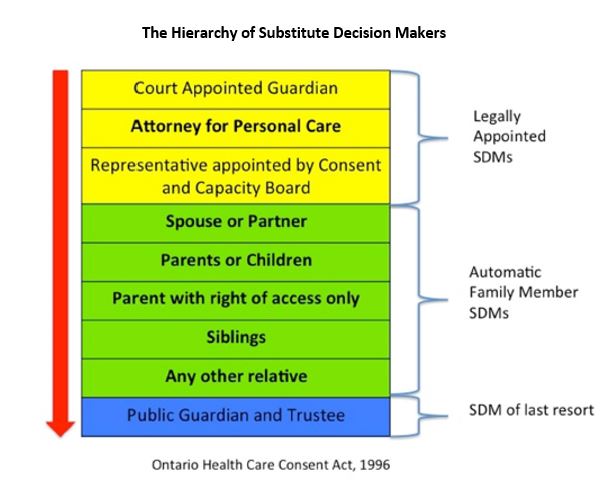
#1 Ask your patients…Have you ever thought about who would be the best person to make decisions on your behalf if you got sick or were too ill to make your own decisions?
Get them thinking about their SDM(s) early to make sure the right person(s) is in the role. Show them the hierarchy, and explain how it works in Ontario. The first step of Advance Care Planning is helping your patients to work through this list, identify their SDM(s) and determine if they need to complete any legal documentation to get anything in place.
#2 Educate…about the role of Substitute Decision Makers?
Help your patients to understand how health care decisions are made in Ontario, and by whom. Explain the role of Substitute Decision Makers (SDMs) … to make decisions on their behalf, the way they would make them and talk about the qualities of a good SDM(s) (e.g. trustworthy, can make difficult decisions, willing to honour your wishes)
#3 Document the SDM(s)…Make note of your patients’ SDM(s) in your records & encourage conversations.
Make sure you have your patients’ SDM(s) information in an easy and accessible place should you ever need to access it quickly. You also want to encourage your patients to talk with their SDM(s) and others about: what is important to them, their wishes, values, beliefs. Conversations are the best way to ensure SDM(s) have the information they need.